
A patient-first approach to scleral contact lenses
By Esther-Simone Visser and Henny Otten from the world-renowned scleral lens specialists, Visser Contactlenzen
Modern scleral lenses are regarded by many as revolutionary. They can prevent the need for corneal transplants, they can bring desperate relief to patients who suffer with dry eyes or cannot close their eye fully, and they can even rescue sight.
It’s amazing how such a small piece of technology can change the lives of patients. We often hear from wearers that scleral lenses have given them their lives back, which is hugely satisfying and a key motivator to keep on making new scientific discoveries and driving innovation in this fascinating area of eye care.
The Visser effect
Scleral lenses offer an incredible design, correcting irregularities of the cornea without touching it and instead, resting on the scleral surface.
They are believed to be one of the earliest types of contact lenses to be manufactured, having existed since the late 19th century. But it was not until almost 100 years later that their popularity became mainstream.
First made from glass and then lightweight plastic around the time of the second world war, early scleral lenses often caused patients to develop corneal edema due to severe hypoxia, which if left untreated can lead to cloudy vision.
It wasn’t until the 1980s that Rients Visser, founder of the famous Visser Contactlenzen practice in the Netherlands, paved the way for scleral lenses with his pioneering work fitting contact lenses. This came after he read a publication from fellow contact lens innovator, Don Ezekiel who described how he used gas permeable materials for scleral lenses.
Rients Visser then focused on improving the design. The 1990s welcomed the introduction of a front-surface cylinder, which improved vision. Visser then made a breakthrough, introducing the back-surface toric scleral lens for his patients that better accommodated the toric nature of the eye.
He continued driving advancement of scleral lenses. In 2010, researchers uncovered new information about the nature of the scleral shape, revealing that they are often tangential rather than curved.1 Rients Visser in collaboration with Bart van der Linden from Menicon, designed and developed bi-tangential shaped scleral lenses. Here, the landing zones (where the lens bears on the sclera) were designed to follow the linear rather than the curved shape of the sclera, and to better accommodate an irregular scleral profile.
These innovative scleral lenses, called Menicon Time XL, have made a huge difference in patient satisfaction and they have improved the popularity of scleral lenses among patients and eye care professionals (ECPs).
4 ways to a patient-first approach with scleral lenses
Scleral lenses are an important front-line tool that should never be underestimated. It’s critical that as ECPs we understand the true potential of scleral lenses, so we can offer them to any patient who will benefit and provide the best care possible.
- Use scleral lenses as an early solution, if indicated. We’re often asked by ECPs how to determine when to prescribe scleral lenses instead of other lenses. Our philosophy is that scleral lenses shouldn’t be seen as a last resort, particularly when keratoconus is concerned. The diagram below shows the guidance we’ve developed to help ECPs choose the right lens for each patient.2
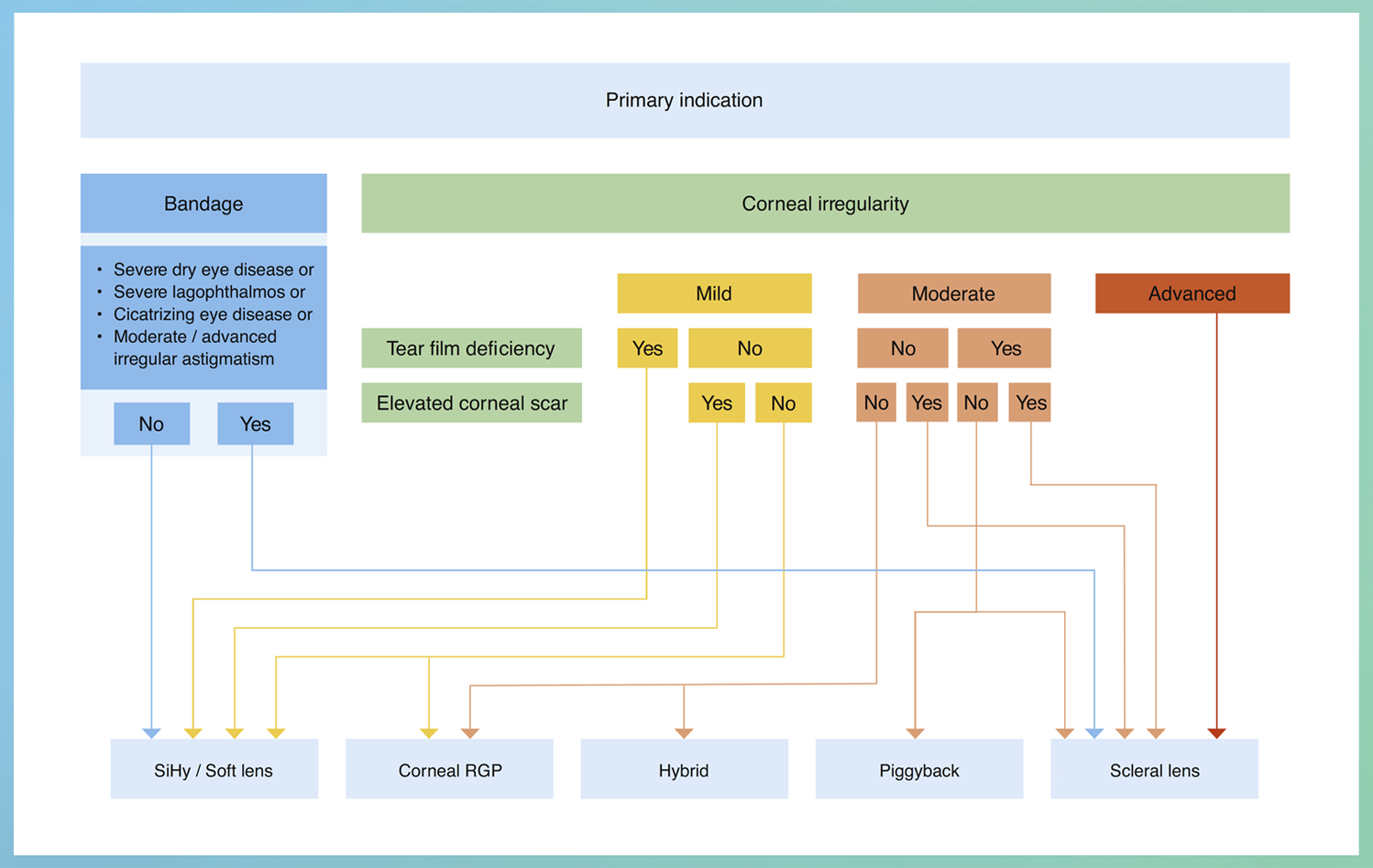
The Visser lens selection algorithm for selecting contact lenses for two principal medical uses: irregular astigmatism and bandage.
• SiHy = silicone hydrogel; RGP = rigid gas-permeable.
• Mild corneal irregularity = acceptable subjective visual quality with SiHy; Moderate corneal irregularity = unacceptable subjective visual quality with SiHy, acceptable lens fit with RGP corneal; Advanced corneal irregularity = unacceptable subjective visual quality with SiHy, no acceptable lens fit with RGP corneal.
• Note: The grading of severe dry eye included grade IV and V based on the Oxford Index for staining and tear film break-up time. SiHy or RGP corneal trial lenses were used to determine the grade of mild”, “moderate”, or “advanced” corneal irregularity.
- Educate the patient from the start. It’s important to provide detail about the lens function and fitting process, what it means to apply and remove them, and the expectations of looking after them early on. This can help with patient independence, while enhancing the ECP-patient relationship. Some patients may be hesitant to wear them but with the right conversations and support, you will reach successful treatment outcomes.
- Make an advanced aftercare plan. Regular check-ups enable the patient to ask questions and allow the ECP to monitor how they’re managing with wearing the lenses. Follow-up visits (or teleconsultations and emails for long distance patients) are critical to help solve any challenges quickly and ensure patients keep persevering with their lenses to ensure successful treatment.
- Get your team onboard. Encourage your staff and colleagues to understand scleral lenses and keep them up-to-date on the latest information with in-office training. Ensure you regularly discuss patient cases across the team to make sure scleral lenses are always considered when suitable.
The Menicon Time XL contact lenses provide a single, compelling solution
The Menicon Time XL contact lens has been designed to make the fitting process simpler for both the patient and ECP, while delivering high performance and comfortable, bespoke scleral lenses for longer daily use.
It is the first mini-scleral lens produced with a bitangential periphery to address the toric shape of the scleral surface seen in 95% of cases. This design optimises the pressure distribution of the lens to improve comfort and allow for longer daily use.1,3 Additionally, it makes the Menicon Time XL lenses suitable for a range of indications, while the adjustable elements ensure it can deliver a scleral lens that’s the perfect fit for patients.
We train our specialists on how to master the Visser fitting method at the Visser Academy, using the philosophy of logical, predictable, and straight-forward fitting. When ECPs are unfamiliar with scleral lenses, fitting them can seem complex but with the right preparation and our structured fitting method it can be a simple and satisfying process.
Additional modifications can be made based on the performance and fitting properties of the diagnostic scleral lens. This way of scleral lens fitting is very accountable – the scleral lens fitter manages the total fitting aspect.
The first step is to identify the scleral profile. The advanced technology necessary to reliably quantify the scleral profile might not be accessible for all ECPs. But the slit lamp is a great instrument here. By using a narrow beam on the superior part of the sclera, the nature of the scleral shape (tangential or curved) can be identified easily.
Next, the lens diameter must be three to five millimetres larger than the horizontal visible iris diameter (HVID). The lens diameter in the diagnostic set is 16mm but lenses are available in a range of diameters from 14 to 17.5mm.
The base curve radius can be adjusted to fit the lens properly. A limbal clearance factor can be used to create more peripheral clearance around the limbal area. Plus, aberration correction and front cylindrical correction can be added on the front surface to improve vision.
The Menicon Time XL lens is produced both linearly and torically and the toric periphery of the lens can be precisely controlled to better align with the sclera for a simple and stable fit. The Menicon Time XL Fitting Guide provides detailed advice on how to fit these lenses in six steps.
![]()
Who can wear scleral lenses?
Scleral lenses are an effective alternative for patients where other optical treatments have failed. Modern scleral lenses provide a fluid reservoir between the cornea and the lens, preventing them from touching the cornea while retaining moisture on the eye. This makes them highly suitable to manage patients with ocular surface disease because the lenses moisten and protect the ocular surface.
Like soft, corneal RGP and other contact lenses, scleral lenses can correct myopia, hyperopia, astigmatism and presbyopia. However, scleral lenses can also neutralise an (advanced) irregular corneal surface and incorporate higher refractive powers which allows them to be used in patients with stronger and more complex refractive conditions.
Scleral lenses have also proven effective in cases when the eyelid isn’t working normally. If a patient cannot close their eyelids, scleral lenses can provide protection for the ocular surface including the cornea, improving sight and quality of life, while reducing discomfort and pain.4 In ptosis cases, the eyelid may droop so much that it covers the pupil and blocks normal vision. Scleral lenses can be used to help keep the eyelid retracted and the eye protected.5
From a practical perspective, scleral lenses can also be a good option for people who take part in contact sports or spend time in dry and dusty environments. Because of their design, scleral lenses are not easily lost and foreign bodies are not easily trapped.6
![]()
We need to guide patients towards this innovative treatment
When patients are diagnosed with an eye disease, they are busy processing their potentially life-changing condition. It’s our job as ECPs to help them find the best possible treatment.
Introducing scleral lenses to patients is the start of a new life-long journey and requires them to form new habits which can take time and patience. But it’s absolutely worth it. Scleral lenses don’t just open up new possibilities for patient vision but for their whole lives.
Authors
Esther-Simone Visser trained at the Hogeschool of Utrecht, The Netherlands, at Moorfields in London, UK and at the University of Houston’s College of Optometry in Houston, Texas. In 2005, she received her Master of Science degree with distinction at City University in London and in 2015, she completed her PhD at the University of Utrecht, The Netherlands. Both research projects were focused on scleral lenses. Her father is Rients Visser.
Henny Otten has been involved in the fitting and development of scleral lenses for more than two decades. He has a passion for sharing his knowledge, instructing new optometrists in the fitting of scleral lenses, and works in several hospitals including two university hospitals where he fits medical lenses. He is also a consultant for Menicon Netherlands.
References
1Van der Worp E. A Guide to Scleral Lens Fitting. Pacific University Common Knowledge: Books and Monographs. 2010. Accessed April 2023.
2Visser ES et al. Objective and subjective evaluation of the performance of medical contact lenses fitted using a contact lens selection algorithm. 2016. Cont Lens Anterior Eye
3Visser, Medical Applications and Outcomes of Bi-tangential Scleral Lenses. Optometry and Vision Science VOL. 90. No.10, October 2013.
4Harthan Jennifer S et al. Therapeutic uses of scleral contact lenses for ocular surface disease: patient selection and special considerations, 2018, Clin Optom
5Katsoulos Konstantinos et al. Scleral contact lenses for the management of complicated ptosis, 2018, Orbit
6ReVision Optometry, 7 Benefits of Scleral Contact Lenses, 2020. Accessed April 2023
